Alzheimer’s Disease & the Gut Microbiome
 For more nutrition and lifestyle medicine webinars and articles, sign up for free at www.nutritank.com.
For more nutrition and lifestyle medicine webinars and articles, sign up for free at www.nutritank.com.
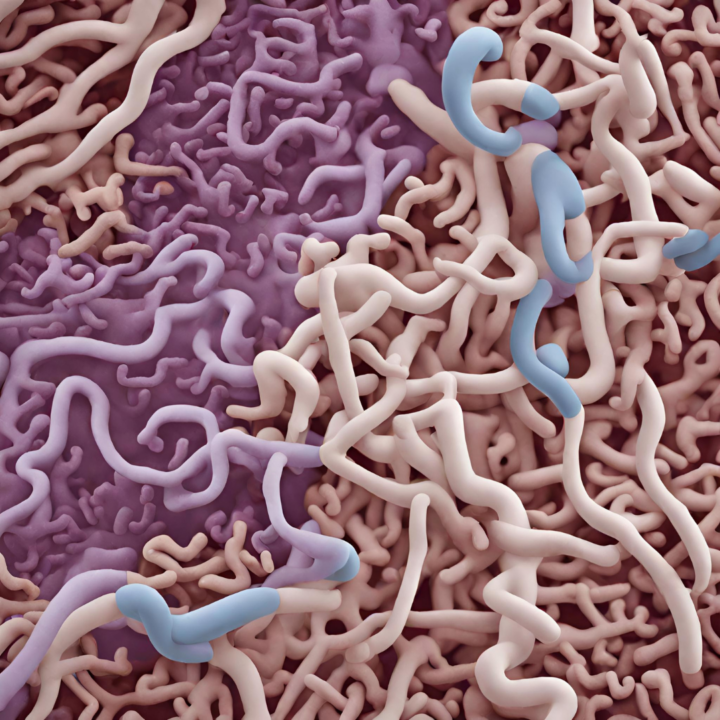
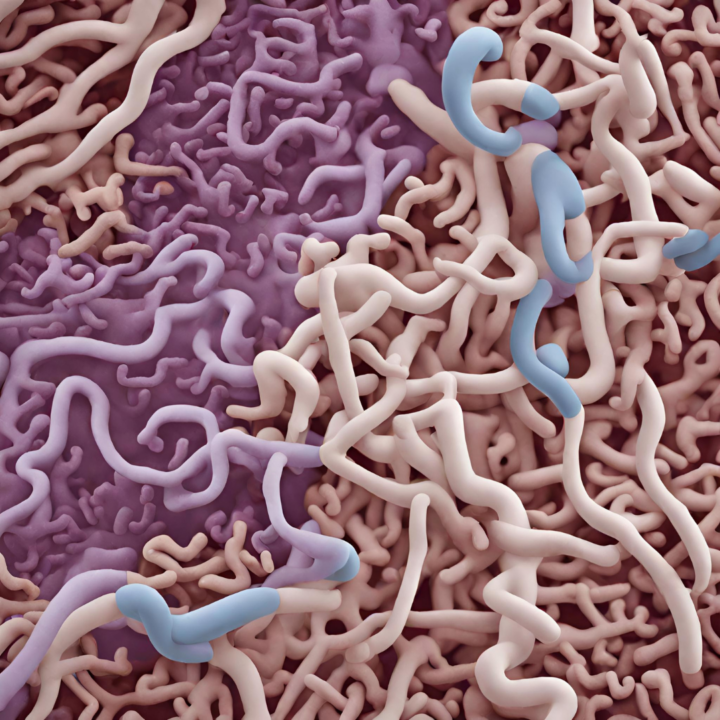
Recent research has demonstrated that changes in gut microbiota may be linked mechanistically to the development of Alzheimer’s disease. The study, which involved a faecal transplant from patients with Alzheimer’s disease and age matched controls into germ free adult rats, demonstrated impairment to behaviours reliant on hippocampal neurogenesis. In this study, patients with Alzheimer’s exhibited lower relative abundance of bacteria associated with healthy ageing (genera Coprococcus), which correlated with lower scores on the Mini-Mental State Examination (MMSE), and an increase in the relative abundance of pathogenic bacteria (genera Desulfovibrio) in patients, which correlated inversely with MMSE scores. Interestingly, the cognitive decline observed in the rats that received gut microbiota from patients with Alzheimer’s disease was independent of amyloid plaque deposition in the brain, suggesting independent mechanisms. This landmark study further demonstrated that symptoms associated with Alzheimer’s symptoms appear to be transferable to healthy young organisms via the gut microbiota (Grabrucker et al., 2023). These findings appear to suggest that gut microbiota dysbiosis may be a key mechanistic causative factor in the pathogenesis of Alzheimer’s disease, and this has been supported by other studies. For example, Hung et al. (2022) reported that patients with Alzheimer’s demonstrate significant increased prevalence of dysbiosis compared with healthy controls. Gut dysbiosis has been shown to promote amyloid-beta aggregation, neuroinflammation, oxidative stress, and insulin resistance, which are key mechanisms in Alzheimer’s disease (Liu et al., 2020).
The future of treating Alzheimer’s disease, for which there is still no known cure, may therefore lie in the gut. An animal study by Sun et al. (2022) has shown that faecal transplant from healthy mice to mice with Alzheimer’s disease can reduce cognitive deficits and alleviate some symptomatology. However, further research is required to explore these findings with relation to human models of Alzheimer’s disease.
Pluta et al. (2020) suggested that personalised diet and interventions could be useful interventions for modulating the gut microbiome and thereby be integrated as treatments for Alzhemer’s disease. This has been supported by various pieces of research over the past five years. Jia et al. (2023) indicated that a healthy diet (involving adherence to the recommended intake of at least 7 of 12 eligible food items, including – fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, and tea) was associated with significant reduction in Alzheimer’s disease risk. Additionally, McEvoy et al. (2017) conducted a study including 5,907 adults, whose dietary patterns were assessed via food frequency questionnaire with relation to cognitive function. Results indicated that individuals who scored higher in terms of more frequent consumption of foods considered part of the MIND diet had a statistically significant better cognitive function (P < 0.001), than those who did not follow this dietary pattern (McEvoy et al. , 2017). A longitudinal study by Morris et al. (2015) including 923 participants, who were followed for 4.5 years and had their diet assessed using a food frequency questionnaire, indicated that adherence to the MIND diet was associated with lower incidence of Alzheimer’s disease.
As research continues to emerge regarding the link between the gut microbiome and Alzheimer’s disease, the importance and relevance of nutrition being included as a key focus in these investigations appears highly merited.
References
Grabrucker, S., Marizzoni, M., Silajdžić, E., Lopizzo, N., Mombelli, E., Nicolas, S., Dohm-Hansen, S., Scassellati, C., Moretti, D. V., Rosa, M., Hoffmann, K., Cryan, J. F., O’Leary, O. F., English, J. A., Lavelle, A., O’Neill, C., Thuret, S., Cattaneo, A., & Nolan, Y. M. (2023). Microbiota from Alzheimer’s patients induce deficits in cognition and hippocampal neurogenesis. Brain : a journal of neurology, awad303. Advance online publication. https://doi.org/10.1093/brain/awad303
Hung CC, Chang CC, Huang CW, Nouchi R, Cheng CH. Gut microbiota in patients with Alzheimer’s disease spectrum: A systematic review and meta-analysis. Aging. 2022;14:477–496.
Jia, J., Zhao, T., Liu, Z., Liang, Y., Li, F., Li, Y., Liu, W., Li, F., Shi, S., Zhou, C., Yang, H., Liao, Z., Li, Y., Zhao, H., Zhang, J., Zhang, K., Kan, M., Yang, S., Li, H., Liu, Z., … Cummings, J. (2023). Association between healthy lifestyle and memory decline in older adults: 10 year, population based, prospective cohort study. BMJ (Clinical research ed.), 380, e072691. https://doi.org/10.1136/bmj-2022-072691
Liu, S., Gao, J., Zhu, M., Liu, K., & Zhang, H. L. (2020). Gut Microbiota and Dysbiosis in Alzheimer’s Disease: Implications for Pathogenesis and Treatment. Molecular neurobiology, 57(12), 5026–5043. https://doi.org/10.1007/s12035-020-02073-3
McEvoy, C. T., Guyer, H., Langa, K. M., & Yaffe, K. (2017). Neuroprotective Diets Are Associated with Better Cognitive Function: The Health and Retirement Study. Journal of the American Geriatrics Society, 65(8), 1857–1862. Available at: <https://doi.org/10.1111/jgs.14922> [Accessed 22/08/2022].
Morris, M. C., Tangney, C. C., Wang, Y., Sacks, F. M., Barnes, L. L., Bennett, D. A., & Aggarwal, N. T. (2015). MIND diet slows cognitive decline with aging. Alzheimer’s & dementia : the journal of the Alzheimer’s Association, 11(9), 1015–1022. Available at:<https://doi.org/10.1016/j.jalz.2015.04.011> [Accessed 22/08/2022]
Sun J, Xu J, Ling Y, et al. Fecal microbiota transplantation alleviated Alzheimer’s disease-like pathogenesis in APP/PS1 transgenic mice. Transl Psychiatry. 2019;9:189.